Although otolaryngologists who regularly inject botulinum toxin into thyroarytenoid muscles for the treatment of spasmodic dysphonia are skilled in performing LEMG, only few have had training in interpreting MUAP signals. And because of the neurophysiological differences between the EMG of big muscles and of muscles of the larynx, even well-trained neuro- physiologists can have difficulties in interpreting LEMG.

Thus, we recommend that a laryngologist and an experienced user with clinical neurophysiology training should work as a team to gain experience with the specific attributes of normal laryngeal muscles.
So first, oral consent, but also a detailed explanation of the intended procedure and expected responses is required. The ability of the patient and willingness to cooperate has to be considered when planning an LEMG examination.
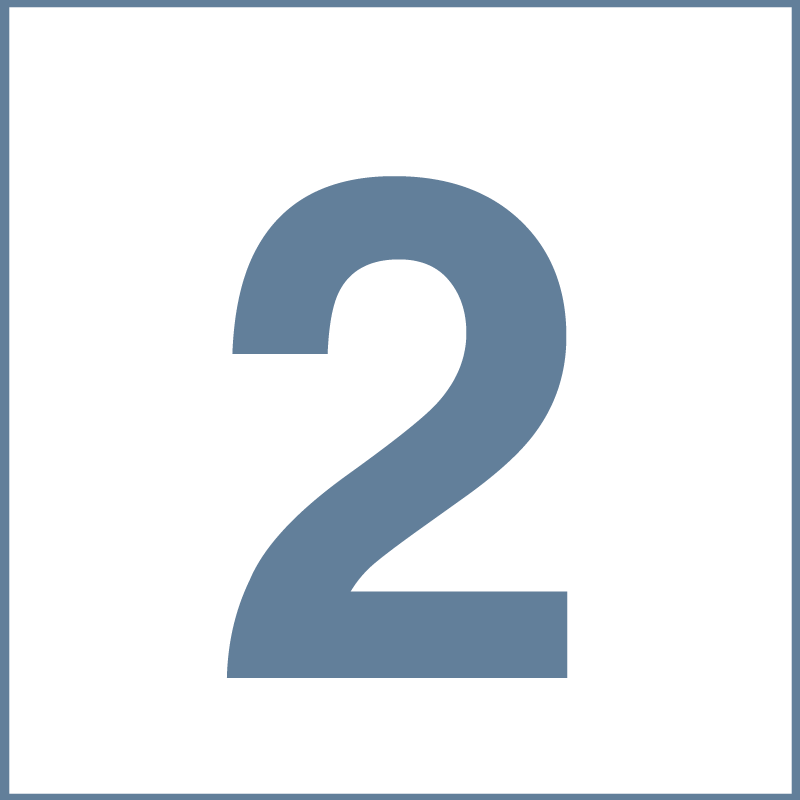
In addition, a detailed examination of the head and neck, including indirect or fiberoptic laryngoscopy and/or videostroboscopy, is important to detect altered anatomy, previous operations, or acute infections—conditions which can potentially hinder the electrode placement.
Bleeding disorders caused, for example, by coagulopathy, warfarin, or acetyl-salicylic acid are relative contraindications. Due to these rare but possible complications, emergency equipment including a cricothyrotomy set must be readily available. As with most medical procedures, LEMG should be carried out only if the medical information expected to be gained justifies the low risk of complications.

Special caution must be exercised in patients with narrow glottic gap due to bilateral vocal cord paralysis. In these cases, LEMG of the vocalis muscle should be performed only on one side at a time. During this test, the respiratory function of the patient must be monitored constantly to prevent breathing problems due to the LEMG.
Electric stimulation studies should not be performed on patients with pacemakers without previous and subsequent cardiologic consultation.

For the LEMG, the patient is asked to adopt a comfortable position with a slightly reclined head. If necessary, the larynx can be anaesthetized locally with lidocaine, either applied transorally to the mucosal surface or with a transcutaneous intraluminal injection.
For transcutaneous insertion with a concentric needle, the patient can be either sitting or supine depending on the patient’s needs and the examiner’s experience.
Hooked-wire electrodes are inserted transorally under visual control with an indirect laryngoscope. Thus, a sitting position of the patient is recommended. A detailed comparison between a transcutaneous and a transoral LEMG follows.
